When Should U Take a Baby to the Hospital With a Fever
Normal body temperature varies from person to person and throughout the solar day. Normal body temperature is highest in children who are preschool aged. Several studies have documented that elevation temperature tends to be in the afternoon and is highest at about 18 to 24 months of historic period when many normal healthy children have a temperature of 101° F. Nevertheless, fever usually is defined as a core body (rectal) temperature ≥ 38.0° C (100.iv° F).
Significance of fever depends on clinical context rather than peak temperature; some minor illnesses cause high fever, whereas some serious illnesses cause only a mild temperature elevation. Although parental assessment is frequently clouded past fear of fever, the history of a temperature taken at home should be considered equivalent to a temperature taken in the role.
Virtually acute fevers in infants and immature children are caused past infection. The most mutual are
-
Viral respiratory or gastrointestinal infections (most common causes overall)
-
Certain bacterial infections (otitis media, pneumonia, urinary tract infections)
However, potential infectious causes of acute fever vary with the kid's historic period. Neonates (infants < 28 days) are considered functionally immunocompromised because they ofttimes fail to comprise infection locally and, as a upshot, are at college hazard of serious invasive bacterial infections almost normally caused past organisms acquired during the perinatal menstruation. The virtually common perinatal pathogens in neonates are group B streptococci, Escherichia coli (and other gram-negative enteric organisms), Listeria monocytogenes Neonatal Listeriosis Neonatal listeriosis is acquired transplacentally or during or subsequently delivery. Symptoms are those of sepsis. Diagnosis is by culture or polymerase chain reaction testing of mother and infant... read more , and canker simplex virus Neonatal Canker Simplex Virus (HSV) Infection Neonatal herpes simplex virus infection is ordinarily transmitted during delivery. A typical sign is vesicular eruption, which may be accompanied by or progress to disseminated illness. Diagnosis... read more  . These organisms tin can cause bacteremia (viremia with herpes simplex), pneumonia Neonatal Pneumonia Neonatal pneumonia is lung infection in a neonate. Onset may be within hours of nascence and office of a generalized sepsis syndrome or after seven days and confined to the lungs. Signs may be express... read more than , pyelonephritis, meningitis Neonatal Bacterial Meningitis Neonatal bacterial meningitis is inflammation of the meninges due to bacterial invasion. Signs are those of sepsis, central nervous system irritation (eg, lethargy, seizures, vomiting, irritability... read more , and/or sepsis Neonatal Sepsis Neonatal sepsis is invasive infection, usually bacterial, occurring during the neonatal flow. Signs are multiple, nonspecific, and include macerated spontaneous activity, less vigorous sucking... read more .
. These organisms tin can cause bacteremia (viremia with herpes simplex), pneumonia Neonatal Pneumonia Neonatal pneumonia is lung infection in a neonate. Onset may be within hours of nascence and office of a generalized sepsis syndrome or after seven days and confined to the lungs. Signs may be express... read more than , pyelonephritis, meningitis Neonatal Bacterial Meningitis Neonatal bacterial meningitis is inflammation of the meninges due to bacterial invasion. Signs are those of sepsis, central nervous system irritation (eg, lethargy, seizures, vomiting, irritability... read more , and/or sepsis Neonatal Sepsis Neonatal sepsis is invasive infection, usually bacterial, occurring during the neonatal flow. Signs are multiple, nonspecific, and include macerated spontaneous activity, less vigorous sucking... read more .
Noninfectious causes of astute fevers include Kawasaki disease Kawasaki Disease Kawasaki affliction is a vasculitis, sometimes involving the coronary arteries, that tends to occur in infants and children between the ages of 1 twelvemonth and eight years. It is characterized past prolonged... read more  , heatstroke, and toxic ingestions (eg, of drugs with anticholinergic effects). Some vaccinations can cause fever either in the start 24 to 48 hours later on the vaccine is given (eg, with pertussis vaccination Diphtheria-Tetanus-Pertussis Vaccine Vaccines that incorporate diphtheria toxoid, tetanus toxoid, and acellular pertussis help protect against diphtheria, tetanus, and pertussis, but they do not forestall all cases. For more than information... read more ) or ane to 2 weeks afterward the vaccine is given (eg, with measles vaccination Measles, Mumps, and Rubella (MMR) Vaccine The measles, mumps, and rubella (MMR) vaccine effectively protects confronting all 3 infections. People who are given the MMR vaccine according to the US vaccination schedule are considered protected... read more ). These fevers typically last from a few hours to a mean solar day. If the child is otherwise well, no evaluation is necessary. Teething does not cause significant or prolonged fevers.
, heatstroke, and toxic ingestions (eg, of drugs with anticholinergic effects). Some vaccinations can cause fever either in the start 24 to 48 hours later on the vaccine is given (eg, with pertussis vaccination Diphtheria-Tetanus-Pertussis Vaccine Vaccines that incorporate diphtheria toxoid, tetanus toxoid, and acellular pertussis help protect against diphtheria, tetanus, and pertussis, but they do not forestall all cases. For more than information... read more ) or ane to 2 weeks afterward the vaccine is given (eg, with measles vaccination Measles, Mumps, and Rubella (MMR) Vaccine The measles, mumps, and rubella (MMR) vaccine effectively protects confronting all 3 infections. People who are given the MMR vaccine according to the US vaccination schedule are considered protected... read more ). These fevers typically last from a few hours to a mean solar day. If the child is otherwise well, no evaluation is necessary. Teething does not cause significant or prolonged fevers.
Potential categories of causes (see Table: Some Mutual Causes of Fever in Children Some Mutual Causes of Fever in Children Normal body temperature varies from person to person and throughout the day. Normal body temperature is highest in children who are preschool aged. Several studies take documented that peak... read more ) include localized or generalized infection, connective tissue illness, and cancer. Miscellaneous specific causes include inflammatory bowel illness Overview of Inflammatory Bowel Disease Inflammatory bowel affliction (IBD), which includes Crohn disease and ulcerative colitis, is a relapsing and remitting condition characterized past chronic inflammation at diverse sites in the gastrointestinal... read more than , diabetes insipidus Central Diabetes Insipidus Diabetes insipidus results from a deficiency of <span course="disableDrug">vasopressin</span> (antidiuretic hormone [ADH]) due to a hypothalamic-pituitary disorder (central... read more with dehydration Dehydration in Children Dehydration is meaning depletion of body h2o and, to varying degrees, electrolytes. Symptoms and signs include thirst, languor, dry mucosa, decreased urine output, and, as the degree... read more , and disordered thermoregulation. Pseudo FUO is likely much more than common than truthful FUO because frequent, small viral disease may exist overinterpreted. In children, despite the numerous possible causes, true FUO is more likely to be an uncommon manifestation of a mutual disease rather than an uncommon affliction; respiratory infections business relationship for well-nigh i one-half of cases of infection-associated FUO.
History of present disease should annotation degree and duration of fever, method of measurement, and the dose and frequency of antipyretics (if any). Important associated symptoms that advise serious illness include poor appetite, irritability, languor, and change in crying (eg, duration, character). Associated symptoms that may suggest the cause include vomiting, diarrhea (including presence of blood or mucus), coughing, difficulty breathing, favoring of an extremity or articulation, and strong or foul-smelling urine. Drug history should be reviewed for indications of drug-induced fever.
Factors that predispose to infection are identified. In neonates, these factors include prematurity, prolonged rupture of membranes, maternal fever, and positive prenatal tests (usually for grouping B streptococcal infections, cytomegalovirus infections, or sexually transmitted diseases). For all children, predisposing factors include recent exposures to infection (including family unit and caregiver infection), indwelling medical devices (eg, catheters, ventriculoperitoneal shunts), recent surgery, travel and environmental exposures (eg, to endemic areas, to ticks, mosquitoes, cats, farm animals, or reptiles), and known or suspected immune deficiencies.
Review of systems should note symptoms suggesting possible causes, including runny nose and congestion (viral upper respiratory infection), headache (sinusitis, Lyme affliction, meningitis), ear hurting or waking in the nighttime with signs of discomfort (otitis media), coughing or wheezing (pneumonia, bronchiolitis), intestinal pain (pneumonia, strep pharyngitis, gastroenteritis, urinary tract infection, abdominal abscess), back hurting (pyelonephritis), and any history of joint swelling or redness (Lyme disease, osteomyelitis). A history of repeated infections (immunodeficiency) or symptoms that suggest a chronic illness, such every bit poor weight gain or weight loss (tuberculosis, cancer), is identified. Certain symptoms tin can help direct the evaluation toward noninfectious causes; they include middle palpitations, sweating, and oestrus intolerance (hyperthyroidism) and recurrent or cyclic symptoms (a rheumatoid, inflammatory, or hereditary disorder).
Past medical history should note previous fevers or infections and known atmospheric condition predisposing to infection (eg, built heart affliction, sickle cell anemia, cancer, immunodeficiency). A family history of an autoimmune disorder or other hereditary conditions (eg, familial dysautonomia, familial Mediterranean fever) is sought. Vaccination history is reviewed to identify patients at take chances of infections that can exist prevented by a vaccine.
Vital signs are reviewed, noting abnormalities in temperature and respiratory rate. In ill-appearing children, claret pressure level should also be measured. Temperature should be measured rectally in infants for accuracy. Any kid with cough, tachypnea, or labored breathing requires pulse oximetry.
The child'southward overall appearance and response to the examination are of import. A febrile child who is overly compliant or listless is of more concern than one who is uncooperative. Withal, an irritable baby or kid who is inconsolable is also of concern. The febrile child who looks quite sick, especially when the temperature has come down, is of great concern and requires in-depth evaluation and continued observation. However, children who announced more comfortable later on antipyretic therapy do not always have a beneficial disorder.
The following findings are of item business:
-
Historic period < one month
-
Lethargy, listlessness, or toxic appearance
-
Respiratory distress
-
Petechiae or purpura
-
Inconsolability
Although serious illness does not always cause loftier fever and many high fevers result from cocky-limited viral infections, a temperature of ≥ 39° C in children < 36 months indicates college risk of serious bacterial infection.
Other vital signs besides are significant. Hypotension should raise business organization most hypovolemia, sepsis, or myocardial dysfunction. Tachycardia in the absence of hypotension may be caused by fever (x to 20 beats/minute increase for each degree above normal) or hypovolemia. An increased respiratory rate may be a response to fever, indicate a pulmonary source of the illness, or be respiratory compensation for metabolic acidosis.
Acute recurrent or periodic fever and chronic fever (FUO Fever of Unknown Origin (FUO) Fever of unknown origin (FUO) is body temperature ≥ 38.3° C (101° F) rectally that does not result from transient and cocky-limited affliction, rapidly fatal disease, or disorders with lucent... read more ) require a high index of suspicion for the many potential causes. However, certain findings can suggest the disorder: aphthous stomatitis, pharyngitis and adenitis (PFAPA syndrome PFAPA Syndrome PFAPA (periodic fevers with aphthous stomatitis, pharyngitis, and adenitis) syndrome is a periodic fever syndrome that typically manifests between ages ii years and five years; it is characterized... read more ); intermittent headaches with runny nose or congestion (sinusitis Sinusitis Sinusitis is inflammation of the paranasal sinuses due to viral, bacterial, or fungal infections or allergic reactions. Symptoms include nasal obstruction and congestion, purulent rhinorrhea... read more  ); weight loss, loftier-run a risk exposure, and night sweats (tuberculosis Tuberculosis (TB) Tuberculosis (TB) is a chronic, progressive mycobacterial infection, often with a menses of latency post-obit initial infection. TB about commonly affects the lungs. Symptoms include productive... read more
); weight loss, loftier-run a risk exposure, and night sweats (tuberculosis Tuberculosis (TB) Tuberculosis (TB) is a chronic, progressive mycobacterial infection, often with a menses of latency post-obit initial infection. TB about commonly affects the lungs. Symptoms include productive... read more  ); weight loss or difficulty gaining weight, heart palpitations, and sweating (hyperthyroidism Hyperthyroidism in Infants and Children Hyperthyroidism is excessive thyroid hormone production. Diagnosis is past thyroid function testing (eg, free serum thyroxine, thyroid-stimulating hormone). Treatment is with <span class="... read more ); and weight loss, anorexia, and night sweats (cancer Overview of Cancer Cancer is an unregulated proliferation of cells. Its prominent properties are A lack of differentiation of cells Local invasion of adjoining tissue Metastasis, which is spread to afar sites... read more ).
); weight loss or difficulty gaining weight, heart palpitations, and sweating (hyperthyroidism Hyperthyroidism in Infants and Children Hyperthyroidism is excessive thyroid hormone production. Diagnosis is past thyroid function testing (eg, free serum thyroxine, thyroid-stimulating hormone). Treatment is with <span class="... read more ); and weight loss, anorexia, and night sweats (cancer Overview of Cancer Cancer is an unregulated proliferation of cells. Its prominent properties are A lack of differentiation of cells Local invasion of adjoining tissue Metastasis, which is spread to afar sites... read more ).
Testing depends on age, appearance of the child, and whether the fever is acute or chronic.
For astute fever, testing for infectious causes is directed by the age of the kid. Typically, children < 36 months, even those who exercise not announced very sick and those who have an apparent source of infection (eg, otitis media), require a thorough search to dominion out serious bacterial infections (eg, meningitis, sepsis). In this age group, early follow-up (past telephone and/or outpatient visit) is important for all those managed at home.
All febrile children < ane month of age require a white blood cell (WBC) count with a manual differential, claret cultures, urinalysis and urine culture (obtained by catheterization, not an external bag) and cerebrospinal fluid (CSF) evaluation with culture and appropriate polymerase chain reaction (PCR) testing (eg, for herpes simplex, enterovirus) as indicated by historical chance factors. Breast x-ray is done in neonates with respiratory manifestations. Stool is sent for culture or enteric PCR stool examination in neonates with diarrhea. Neonates are hospitalized and given empiric 4 antibody coverage for the most common neonatal pathogens (eg, using ampicillin and gentamicin or ampicillin and cefotaxime); antibiotics are continued until blood, urine, and CSF cultures take been negative for 48 hours. Acyclovir also should exist given if neonates are sick-appearing, take mucocutaneous vesicles, have onset of disease at about 2 weeks of age, take a maternal history of genital canker simplex virus (HSV) infection, or take seizures; acyclovir is stopped if results of CSF HSV PCR testing are negative.
Delirious children between 1 calendar month and 3 months of age require a different approach, which has evolved over the terminal few decades because the number of children in this age grouping who plough out to have a potentially serious bacterial infection has been markedly reduced by routine immunization against H. influenzae type b and S. pneumoniae. Clinicians must nonetheless maintain vigilance because, although serious bacterial infections take been reduced, they accept not been eliminated. Therefore, clinicians who choose to notice without treatment or ship home under parental observation need to have a greater certainty regarding that child's low-chance condition than that of a child who is tested, admitted, and treated.
Infants in this 29- to 90-day age group are differentiated based on
-
Temperature
-
Clinical appearance
-
Laboratory results
Typically, all infants 29 to threescore days of age and infants 61 to 90 days of age who are ill-actualization or with risk factors for serious bacterial infection (eg, significant congenital anomalies, prematurity, technology dependence, unvaccinated) should have a WBC count with a transmission differential, claret cultures, urinalysis and urine culture (obtained past catheterization, not an external bag), and lumbar puncture with CSF evaluation, including civilization. Chest ten-ray is washed in those with respiratory manifestations, and stool is sent for stool civilization or enteric PCR stool test in those with diarrhea. Some experts may defer WBC count and blood culture in well-actualization delirious infants 61 to 90 days of age without risk factors for serious bacterial infection pending urinalysis results. Lumbar puncture can be deferred in infants aged 61 to 90 days who appear well, take a rectal temperature < 38.v° C, have a normal urinalysis and a normal WBC count (5,000 to 15,000/mcL [5 to 15 × x9/50]) if done, and who take knowledgeable caregivers, reliable transportation, and well-established follow-upwardly; some experts as well defer CSF testing in like well-appearing infants aged 29 to 60 days, although there are no firm guidelines regarding minimum necessary testing in this age group.
Infants between 1 month and 3 months of historic period with a documented respiratory syncytial virus (RSV) or flu infection appear to have a markedly reduced risk of serious bacterial infection, which some experts believe permits modifications to the higher up recommendations. Well-appearing delirious infants in this historic period group with RSV bronchiolitis, or with influenza documented by PCR testing during a period of high seasonal prevalence and who have normal urinalysis results, do non necessarily crave blood or CSF studies or empiric antibiotics. Children with abnormal urinalysis results, specially those betwixt 29 days and 60 days of age, warrant additional laboratory evaluation and management as described below.
Febrile infants betwixt one month and 3 months who are ill-appearing, have an abnormal weep, or have rectal temperature ≥ 38.v° C have a high risk of serious bacterial infection regardless of initial laboratory results. Such infants should be hospitalized and given empiric antibody therapy using ceftriaxone or cefotaxime awaiting the results of blood, urine, and CSF cultures.
Well-appearing infants between 1 month and 3 months with CSF pleocytosis, an abnormal urinalysis or chest x-ray, or a peripheral WBC count ≤ 5,000/mcL (≤ 5 × 109/Fifty) or ≥ 15,000/mcL (≥ xv × x9/L) should be admitted to the infirmary for handling with age-specific empiric antibiotics as described above. If empiric antibiotics are to exist given, CSF analysis should be strongly considered (if not already done) especially in infants 29 to lx days of age.
Well-appearing febrile infants between one month and three months with a rectal temperature < 38.5° C and a normal WBC count and urinalysis (and CSF analysis and chest x-ray, if done) are at low take chances of serious bacterial infections. Such infants can be managed every bit outpatients if reliable follow-upward is bundled within 24 hours either by phone or past return visit, at which time preliminary culture results are reviewed. If the family's social state of affairs suggests that follow-upwardly within 24 hours is problematic, infants should be admitted to the hospital and observed. If infants are sent home, any deterioration in clinical status or worsening of fever, a positive blood civilisation non thought to be a contaminant, or a positive urine culture in an infant who remains febrile warrants immediate hospitalization with echo cultures and age-specific empiric antibiotic therapy as described above.
Febrile children between 3 months and 36 months of age who have an apparent source of fever on examination and who practice not appear ill or toxic can exist managed based on this clinical diagnosis. Children who are ill-appearing should be fully evaluated for serious bacterial infection with WBC count, cultures of blood, urine, and, when meningitis is suspected, CSF. Those with tachypnea or a WBC count > xx,000/mcL (> 20 × 109/50) should have a chest 10-ray. These children should be given parenteral antibiotic therapy (commonly using ceftriaxone) targeting the probable pathogens in this historic period group (S. pneumoniae, Staphylococcus aureus, Neisseria meningitidis, H. influenzae type b) and be admitted to the hospital pending culture results.
Well-appearing children in this historic period group who have a temperature > 39° C and no identifiable source on examination (fever without source) and who are non fully immunized take a risk of occult bacteremia as high equally five% (equal to the chance before the pneumococcal and H. influenzae conjugate vaccines came into use). These children should have a CBC with differential, blood civilization, and urinalysis and urine culture. A chest ten-ray should be done if the WBC count is ≥ 20,000/mcL (> twenty × tennine/L) . Children who have a WBC count ≥ 15,000/mcL (≥ xv × ten9/50) should be given parenteral antibiotics pending blood and urine culture results. Ceftriaxone (50 mg/kg IM) is preferred considering of its wide antimicrobial spectrum and prolonged duration of activity. Children who received parenteral antibiotics should have follow-upwards within 24 hours by telephone or by return visit, at which time preliminary culture results are reviewed. If the social situation suggests that follow-upwards within 24 hours is problematic, children should be admitted to the hospital. Children who are non treated with antibiotics should be brought for reevaluation if they are still delirious (≥ 38° C) after 48 hours or earlier if they become sicker or if new symptoms or signs develop.
For well-appearing children who accept a temperature > 39° C and fever without source and who are completely immunized, risk of bacteremia is < 0.v%. At this low-take chances level, most laboratory testing and empiric antibody therapy are neither indicated nor price-effective. However, considering urinary tract infection (UTI) tin can be an occult source of infection in fully immunized children in this age group, girls < 24 months, circumcised boys < 6 months, and uncircumcised boys < 12 months should accept a urinalysis and urine culture (obtained by catheterization, not an external handbag) and be appropriately treated if UTI is detected. For other completely immunized children, urine testing is done but when they have symptoms or signs of UTI, they have a prior history of UTI or urogenital anomalies, or fever has lasted > 48 hours. For all children, caregivers are instructed to return immediately if fever becomes higher, the child looks sicker, or new symptoms or signs develop.
For febrile children > 36 months, testing is directed by history and examination. In this historic period group, a child's response to serious illnesses is sufficiently adult to exist recognized clinically (eg, nuchal rigidity is a reliable finding of meningeal irritation), so empiric testing (eg, screening WBC counts, urine and blood cultures) is not indicated.
For astute recurrent or periodic fever, laboratory tests and imaging should be directed toward likely causes based on findings from the history and physical test. PFAPA syndrome PFAPA Syndrome PFAPA (periodic fevers with aphthous stomatitis, pharyngitis, and adenitis) syndrome is a periodic fever syndrome that typically manifests between ages 2 years and 5 years; it is characterized... read more should be considered in young children who accept periodic high fever at intervals of most 3 to v weeks with aphthous ulcers, pharyngitis, and/or adenitis. Betwixt episodes and even during the episodes, the children announced healthy. Diagnosis requires 6 months of stereotypic episodes, negative throat cultures during episodes, and exclusion of other causes (eg, specific viral infections). In patients with attacks of fever, arthralgia, peel lesions, oral cavity ulcers, and diarrhea, IgD levels should be measured to wait for hyperimmunoglobulinemia D syndrome (HIDS). Laboratory features of HIDS include elevated C-reactive poly peptide (CRP) and erythrocyte sedimentation charge per unit (ESR) and markedly elevated IgD (and often IgA). Genetic testing is available for familial Mediterranean fever (FMF), TNF receptor–associated periodic syndrome (TRAPS), and HIDS.
For chronic fever (fever of unknown origin [FUO]), laboratory tests and imaging should be directed toward probable causes of fever based on the patient's age and findings from the history and concrete test. Indiscriminate ordering of laboratory tests is unlikely to be helpful and tin can exist harmful (ie, because of adverse effects of unnecessary confirmatory testing of false positives). The pace of the evaluation is dictated by the appearance of the kid. The pace should be rapid if the kid is sick-actualization, merely can exist more deliberate if the child appears well.
All children with FUO should have
-
Complete blood count (CBC) with manual differential
-
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP)
-
Claret cultures
-
Urinalysis and urine culture
-
Chest x-ray
-
Serum electrolytes, claret urea nitrogen (BUN), creatinine, albumin, and hepatic enzymes
-
HIV serology
-
Tuberculin skin test (PPD)
The results of these studies in conjunction with findings from the history and physical examination can focus further diagnostic tests.
Anemia may exist a clue to malaria, infective endocarditis, inflammatory bowel disease, systemic lupus erythematosus, or tuberculosis (TB). Thrombocytosis is a nonspecific acute-phase reactant. The total WBC count and the differential generally are less helpful, although children with an accented neutrophil count > 10,000/mcL (> 10 × 109/Fifty) accept a higher run a risk of serious bacterial infection. If atypical lymphocytes are present, a viral infection is likely. Immature WBCs should prompt further evaluation for leukemia Diagnosis Acute lymphoblastic leukemia (ALL) is the well-nigh common pediatric cancer; it also strikes adults of all ages. Malignant transformation and uncontrolled proliferation of an abnormally differentiated... read more than 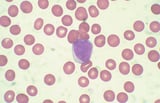 . Eosinophilia may be a clue to parasitic, fungal, neoplastic, allergic, or immunodeficiency disorders.
. Eosinophilia may be a clue to parasitic, fungal, neoplastic, allergic, or immunodeficiency disorders.
Blood cultures should exist done in all patients with FUO at least once and more than often if suspicion of serious bacterial infection is high. Three blood cultures should be done over 24 hours in patients who have any manifestations of infective endocarditis. A positive claret civilisation, particularly for S. aureus, should raise suspicion for occult skeletal or visceral infection or endocarditis and lead to operation of a bone scan and/or echocardiography.
Other tests are done selectively based on findings:
-
Stool testing
-
Bone marrow test
-
Serologic testing for specific infections
-
Testing for connective tissue and immunodeficiency disorders
-
Imaging
Stool cultures or test for ova and parasites may be warranted in patients with loose stools or contempo travel. Salmonella enteritis can infrequently manifest as FUO without diarrhea.
Bone marrow examination in children is most useful in diagnosing cancer (specially leukemia) or other hematologic disorders (eg, hemophagocytic disease) and may exist warranted in children with otherwise unexplained hepatosplenomegaly, lymphadenopathy, or cytopenias.
Serologic testing that may be warranted, depending on the instance, includes but is not limited to Epstein-Barr virus infection, cytomegalovirus infection, toxoplasmosis, bartonellosis (cat-scratch disease), syphilis, and certain fungal or parasitic infections.
An antinuclear antibody (ANA) examination should be washed in children > five years with a strong family history of rheumatologic affliction. A positive ANA examination suggests an underlying connective tissue disorder, specially systemic lupus erythematosus. Immunoglobulin levels (IgG, IgA, and IgM) should be measured in children with a negative initial evaluation. Low levels may indicate an immunodeficiency. Elevated levels tin occur in chronic infection or an autoimmune disorder.
Imaging of the nasal sinuses, mastoids, and gastrointestinal tract should exist done initially only when children accept symptoms or signs related to those areas but may be warranted in children in whom FUO remains undiagnosed afterward initial testing. Children with elevated ESR or CRP, anorexia, and weight loss should have studies to exclude inflammatory bowel disease Diagnosis Crohn disease is a chronic transmural inflammatory bowel illness that usually affects the distal ileum and colon merely may occur in whatever part of the alimentary canal. Symptoms include diarrhea... read more  , particularly if they also have abdominal complaints with or without anemia. Yet, imaging of the gastrointestinal tract should be washed eventually in children whose fevers persist without other explanation and may be caused by disorders such every bit psoas abscess or cat-scratch disease. Ultrasonography, CT, and MRI can be useful in evaluating the abdomen and can detect abscesses, tumors, and lymphadenopathy. Imaging of the primal nervous system is by and large not helpful in the evaluation of children with FUO. However, lumbar puncture may be warranted in children with persistent headache, neurologic signs, or an indwelling ventriculoperitoneal shunt. Other imaging techniques, including os scan or tagged WBC browse, can be helpful in selected children whose fevers persist without other explanation when suspicion for a source that could be detected by these tests exists. Ophthalmologic test by slit lamp is useful in some patients with FUO to look for uveitis (eg, every bit occurs in juvenile idiopathic arthritis) or leukemic infiltration. Biopsy (eg, of lymph nodes or liver) should be reserved for children with evidence of involvement of specific organs.
, particularly if they also have abdominal complaints with or without anemia. Yet, imaging of the gastrointestinal tract should be washed eventually in children whose fevers persist without other explanation and may be caused by disorders such every bit psoas abscess or cat-scratch disease. Ultrasonography, CT, and MRI can be useful in evaluating the abdomen and can detect abscesses, tumors, and lymphadenopathy. Imaging of the primal nervous system is by and large not helpful in the evaluation of children with FUO. However, lumbar puncture may be warranted in children with persistent headache, neurologic signs, or an indwelling ventriculoperitoneal shunt. Other imaging techniques, including os scan or tagged WBC browse, can be helpful in selected children whose fevers persist without other explanation when suspicion for a source that could be detected by these tests exists. Ophthalmologic test by slit lamp is useful in some patients with FUO to look for uveitis (eg, every bit occurs in juvenile idiopathic arthritis) or leukemic infiltration. Biopsy (eg, of lymph nodes or liver) should be reserved for children with evidence of involvement of specific organs.
Empiric handling with anti-inflammatory drugs or antibiotics should not be used as a diagnostic measure except when juvenile idiopathic arthritis is suspected; in such cases, a trial of nonsteroidal anti-inflammatory drug (NSAIDs) is the recommended starting time-line therapy. Response to anti-inflammatory drugs or antibiotics does not assistance distinguish infectious from noninfectious causes. As well, antibiotics can cause false-negative cultures and mask or filibuster the diagnosis of important infections (eg, meningitis, parameningeal infection, endocarditis, osteomyelitis).
Treatment is directed at the underlying disorder.
Fever in an otherwise healthy child does not necessarily require treatment. Although antipyretics can provide condolement, they do not change the form of an infection. In fact, fever is an integral part of the inflammatory response to infection and can help the child fight the infection. However, most clinicians utilize antipyretics to help alleviate discomfort and to reduce physiologic stresses in children who have cardiopulmonary disorders, neurologic disorders, or a history of febrile seizures.
Antipyretic drugs that are typically used include
-
Acetaminophen
-
Ibuprofen
Acetaminophen tends to be preferred because ibuprofen decreases the protective effect of prostaglandins in the tum and, if used chronically, can lead to gastritis. Epidemiologic studies have suggested a possible clan between the development of asthma and maternal and infant use of acetaminophen and ibuprofen. A randomized drug trial comparing the two showed that these drugs in usual doses do not lead to worsening of existing asthma (1 Treatment reference Normal trunk temperature varies from person to person and throughout the solar day. Normal body temperature is highest in children who are preschool aged. Several studies have documented that peak... read more than ). However, the question remains whether the use of these drugs during pregnancy or early childhood increases the risk of developing asthma. If used, the dosage of acetaminophen is 10 to 15 mg/kg orally, IV, or rectally every 4 to 6 hours. The dosage of ibuprofen is ten mg/kg orally every 6 hours. Employ of 1 antipyretic at a fourth dimension is preferred. Some clinicians alternate the ii drugs to treat high fever (eg, acetaminophen at six AM, 12 PM, and half dozen PM and ibuprofen at 9 AM, 3 PM, and 9 PM), but this approach is not encouraged considering caregivers may become confused and inadvertently exceed the recommended daily dose. Aspirin should be avoided in children because it increases the risk of Reye syndrome Reye Syndrome Reye syndrome is a rare form of acute encephalopathy and fatty infiltration of the liver that tends to occur later some astute viral infections, peculiarly when salicylates are used. Diagnosis... read more if certain viral illnesses such equally influenza and varicella are present.
Nondrug approaches to fever include putting the child in a warm or tepid bath, using cool compresses, and undressing the kid. Caregivers should exist cautioned not to use a cold water bath, which is uncomfortable and which, past inducing shivering, may paradoxically elevate body temperature. As long as the temperature of the water is slightly libation than the temperature of the child, a bath provides temporary relief.
-
1. Sheehan WJ, Mauger DT, Paul IM, et al: Acetaminophen versus ibuprofen in immature children with mild persistent asthma. N Engl J Med 375(7):619–630, 2016. doi: ten.1056/NEJMoa1515990.
-
Most acute fever is caused by viral infections.
-
Causes and evaluation of acute fever differ depending on the age of the child.
-
A small but real number of children < 36 months with fever without localizing signs (primarily those who are incompletely immunized) can have pathogenic bacteria in their bloodstream (occult bacteremia) and be early in the course of a potentially life-threatening infection.
-
Teething does not cause pregnant fever.
-
Antipyretics exercise non change the outcome just may make children experience better.
Source: https://www.msdmanuals.com/professional/pediatrics/symptoms-in-infants-and-children/fever-in-infants-and-children
0 Response to "When Should U Take a Baby to the Hospital With a Fever"
Enviar um comentário